Medical Devices and Remote Healthcare: Empowering Pharmacists in the Digital Era
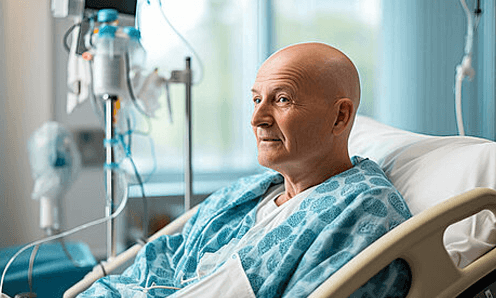
The rise of remote patient monitoring and the use of smart medical devices such as AR (augmented reality) and VR (virtual reality) have revolutionized how pharmacists and healthcare professionals engage with patients. These technologies enable remote consultations, real-time monitoring, and more personalized medication management—without requiring physical visits.
How Do Modern Medical Devices Help Pharmacists?
Pharmacists can now conduct virtual counseling, demonstrate medication usage through immersive VR tools, and receive real-time biometric data like blood pressure, glucose levels, and oxygen saturation directly from wearable or connected devices. This data-driven model helps them make accurate dosage recommendations and intervene promptly in critical situations.
Key Benefits for Pharmacists:
-
Remote chronic disease management (diabetes, hypertension).
-
Efficient follow-up for elderly or mobility-challenged patients.
-
Enhanced patient counseling through interactive, immersive environments.
-
Reduced clinic loads and minimized unnecessary in-person visits.
FAQs
What types of medical devices are most commonly used in remote care?
Wearables, blood pressure monitors, glucose monitors, and AR/VR tools are widely used in telepharmacy and remote patient monitoring.
How can pharmacists integrate remote care into their workflow?
By using smart apps and connected devices, pharmacists can track treatment adherence, conduct virtual consultations, and collaborate with physicians seamlessly.